3. Deaths from COVID-19 or related to another cause
The criteria for attributing a death to COVID-19 vary between countries and data sources, including biological tests, clinical diagnoses, or a reference to the infection on the death certificate. Patients dying at hospital were generally tested earlier, on admission, while deaths at home or at socio-medical institutions may be qualified in various manners. Consequently, the COVID-19 death count may vary from one country to the next according to the criteria used to attribute cause of death to COVID-19.
References to COVID-19 may be counted by analyzing death certificates listing the medical causes leading to death. COVID-19 may be the main (or initial) cause or combined with other pathologies. Analyses at hospitals demonstrate a higher risk of death for those with multiple concurrent diseases. This result is also consistent with the increased risk of COVID-19 fatalities for older individuals (with age also increasing the risk of multi-morbidity) and for men.
Establishing statistics on the causes of death is a lengthy process, with only a part of the required data being available rapidly. This includes the electronic transmission of medical certificates of death, available in the UK and France. For the French epidemiology review of the situation at 21 April 2020, in the early days of the epidemic, just over 7,500 electronic certificates of death attributed the cause of death to COVID-19. While these partial data may shed initial light on the epidemiological profile of the dead, COVID-19 mortality based on medical certificates of death may be analyzed in depth only once all the certificates have been obtained and processed.
Another approach to mortality during the epidemic consists in using the declarations of death transmitted to national statistics institutes, with no identification of the cause.
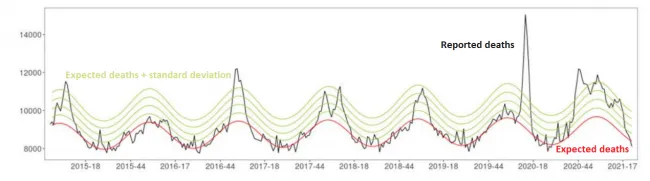
While deaths directly linked to COVID-19 may not be identified using this source, we can estimate the excess mortality reported during the epidemic (Pison, Meslé, “The Conversation”). In France, the weekly death rates published by the National Institute of Statistics and Economic Studies (INSEE), clearly show annual peaks in mortality corresponding to flu epidemics (Figure 3.1). From January to mid-March 2020, weekly mortality did not exceed that of the previous year owing to a mild seasonal flu epidemic. Mortality rates were lower than in 2017 and 2018, when the flu epidemic caused more deaths. But from 16 March onwards, mortality considerably exceeded that of previous years. Over 76,000 deaths, all causes combined, occurred between 16 March and 6 April, compared with 63,700 for the same period in 2019 and 71,000 in 2018 (INSEE). The figure also clearly shows the excess mortality at the end of 2020 and the start of 2021. Though peaking less than in March-April, excess mortality persisted for a much longer period.
Thus far, we have not been able to determine in this excess mortality the share of deaths directly attributable to COVID-19 (main cause), the share of deaths to which COVID-19 contributed (by weakening the organism), or the share of deaths related to other causes, stemming notably from the lockdown. While some causes, such as road accidents, decreased, forgoing or postponing health visits may have worsened the state of health of some individuals and increased mortality by other causes during the period. It will be possible to analyze these aspects in detail once the statistics of causes of death have been made public.